How bad do nose jobs hurt? This question is paramount for anyone considering rhinoplasty. Understanding the pain levels associated with this procedure, from initial consultation to post-operative recovery, is crucial for informed decision-making. This exploration delves into the various factors influencing pain perception, including individual tolerance, surgical techniques, and post-operative care strategies. We’ll examine the typical pain experience throughout the process, offering insights into pain management techniques and realistic expectations for recovery.
Rhinoplasty, or a nose job, involves reshaping the nasal bones and cartilage to alter the nose’s appearance. The level of pain experienced varies greatly depending on several factors, including the complexity of the surgery, the individual’s pain tolerance, and the effectiveness of pain management strategies. This detailed analysis aims to provide a comprehensive understanding of the pain associated with rhinoplasty, empowering prospective patients to make informed choices and manage their expectations.
Pain Levels During Rhinoplasty
Rhinoplasty, or a nose job, is a surgical procedure that can significantly alter the appearance of the nose. While the results are often highly desirable, understanding the potential for pain and discomfort throughout the process is crucial for patient preparation and realistic expectations. Pain levels vary significantly depending on individual pain tolerance, the specific surgical technique employed, and the post-operative care received.
Pain Levels During Different Stages of Rhinoplasty
Pain experienced during rhinoplasty is generally manageable. Pre-operative anxiety can contribute to perceived discomfort, although this is typically addressed through pre-operative consultations and medication. During the surgery itself, the patient is under general anesthesia and experiences no pain. Post-operative pain is the most significant concern, usually peaking within the first 24-48 hours. This pain is often described as pressure, throbbing, or aching, localized to the nose and surrounding areas.
The intensity varies considerably among individuals; some report mild discomfort manageable with over-the-counter analgesics, while others may require stronger prescription pain medication. The pain typically diminishes gradually over the following days and weeks.
Pain Management Techniques and Their Effectiveness
Effective pain management is a critical component of rhinoplasty recovery. Pre-operative consultations typically include a discussion of pain management strategies. These strategies often involve a combination of approaches. Prescription pain medications, such as opioids or NSAIDs, are frequently prescribed to manage post-operative pain. Ice packs applied to the nose can help reduce swelling and alleviate discomfort.
Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can be used to supplement prescription medications or for managing milder pain. In some cases, nerve blocks may be used to provide additional pain relief during the immediate post-operative period. The effectiveness of these techniques varies depending on individual responses and the severity of the pain.
Comparison of Pain Levels in Open vs. Closed Rhinoplasty Techniques
Open and closed rhinoplasty are two common surgical techniques. While both procedures can result in similar aesthetic outcomes, the post-operative pain experience may differ slightly. Open rhinoplasty, which involves an incision across the columella (the fleshy area between the nostrils), is often associated with slightly more post-operative swelling and bruising, potentially leading to increased discomfort in the initial recovery phase.
Closed rhinoplasty, which involves making incisions inside the nostrils, generally results in less visible scarring and potentially less post-operative pain and swelling. However, the difference in pain levels is often subtle and not universally experienced.
Pain Level Rating Scale
A subjective pain scale, such as the 0-10 numerical rating scale (NRS), is often used to assess post-operative pain. 0 represents no pain, while 10 represents the worst imaginable pain. The patient’s individual pain tolerance significantly influences their perception of pain intensity. For example, a patient with a high pain tolerance might rate a moderate level of pain as a 4 on the NRS, while a patient with a low pain tolerance might rate the same pain as a 7.
This emphasizes the importance of open communication between the patient and their surgeon regarding pain management strategies. Accurate pain assessment allows for individualized treatment plans to optimize post-operative comfort.
Factors Influencing Pain Perception: How Bad Do Nose Jobs Hurt
Pain experienced after rhinoplasty is subjective and varies significantly among individuals. Several factors interact to influence the intensity and duration of post-operative discomfort. Understanding these factors can help patients manage expectations and potentially mitigate pain.Individual pain tolerance significantly impacts the perception of rhinoplasty pain. Pain tolerance is a complex interplay of genetic predisposition, psychological factors, and past experiences with pain.
A person with a naturally high pain tolerance may experience post-operative discomfort as mild, while an individual with low pain tolerance may perceive the same level of stimulation as significantly more painful. This inherent difference is not a reflection of strength or weakness but rather a biological variation.
The Role of Anxiety and Stress in Amplifying Pain Perception
Anxiety and stress before and after surgery can substantially amplify pain perception. The body’s stress response releases hormones like cortisol, which can sensitize nerve endings and increase the perception of pain. Pre-operative anxiety, stemming from fear of the unknown or the surgical procedure itself, can heighten the pain experienced post-operatively. Similarly, post-operative stress related to recovery, potential complications, or changes in appearance can exacerbate pain.
The pain experienced after a rhinoplasty varies greatly among individuals, influenced by factors such as surgical technique and individual pain tolerance. For a different kind of aesthetic consideration, choosing the right accessories can dramatically alter an outfit’s impact; for instance, consider the advice on pairing accessories with a royal blue dress found in this helpful guide: cobalt blue how to accessorize a royal blue dress.
Returning to rhinoplasty, post-operative discomfort is usually manageable with prescribed medication, and the overall healing process typically takes several weeks.
Effective pre-operative counseling and pain management strategies can help mitigate this effect.
Influence of Pre-existing Medical Conditions
Certain medical conditions can influence an individual’s pain response to surgery. For example, patients with fibromyalgia, a chronic pain condition, may experience heightened sensitivity to pain stimuli, making post-operative discomfort more intense. Similarly, individuals with chronic pain syndromes or nerve damage may have a lower pain threshold and a greater susceptibility to prolonged pain after rhinoplasty. These pre-existing conditions need to be carefully considered during pre-operative assessment and pain management planning.
Impact of Medication and Anesthesia on Pain Levels
Medication and anesthesia play a crucial role in managing pain after rhinoplasty. The type and dosage of anesthetic used during the procedure, as well as the post-operative analgesic regimen, significantly affect pain levels. Local anesthesia numbs the surgical site during the procedure, while general anesthesia renders the patient unconscious. Post-operative pain management typically involves a combination of prescription pain relievers, such as opioids or NSAIDs, and potentially other medications to address swelling and inflammation.
The effectiveness of these medications can vary depending on individual factors, including metabolism and potential drug interactions. Careful consideration of these factors is necessary to tailor the most effective pain management plan for each patient.
Post-Operative Discomfort and Recovery
Rhinoplasty, while transformative, involves a period of post-operative recovery characterized by varying levels of discomfort. Understanding the typical symptoms, their progression, and effective management strategies is crucial for a smooth recovery. This section details the expected discomfort, provides a timeline for pain reduction, and Artikels self-care techniques to minimize post-operative challenges.Post-operative symptoms following rhinoplasty primarily involve pain, swelling, and bruising.
Pain is usually described as mild to moderate, often localized to the nose and surrounding areas. The intensity and duration of pain vary significantly among individuals, influenced by factors such as the complexity of the surgery, individual pain tolerance, and adherence to post-operative instructions. Swelling is a common and expected occurrence, peaking around 2-3 days post-surgery and gradually subsiding over several weeks.
Bruising, if present, typically appears around the eyes and cheeks and resolves within 1-2 weeks. Other common symptoms include nasal congestion, headaches, and occasional numbness or tingling in the nose and upper lip.
Pain Timeline Following Rhinoplasty
The pain experienced after rhinoplasty generally follows a predictable pattern. Immediately following surgery, patients may experience moderate discomfort, often well-managed with prescribed pain medication. Pain levels typically peak within the first 24-48 hours and then gradually decrease. By day 3-5, most patients report a significant reduction in pain, requiring less medication. By the end of the first week, pain is usually minimal, though some residual discomfort or pressure may persist.
Significant pain beyond the first week should be reported to the surgeon. For example, a patient might experience a 7 out of 10 pain score on a visual analogue scale (VAS) immediately post-op, dropping to a 3/10 by day 2, a 1/10 by day 5, and negligible pain by day 7. This is a general guideline; individual experiences may vary.
Self-Care Strategies for Pain and Swelling Management
Managing post-operative pain and swelling effectively contributes to a faster and more comfortable recovery. Several self-care strategies can be implemented:
Several self-care strategies are crucial for managing post-operative pain and swelling. These include:
- Medication: Adhering strictly to the prescribed pain medication regimen is vital. This often involves taking medication as directed, even if pain is minimal, to prevent discomfort from escalating.
- Ice Packs: Applying ice packs to the nose and surrounding areas for 15-20 minutes at a time, several times a day, helps reduce swelling and numb the area.
- Elevation: Keeping the head elevated on extra pillows during sleep reduces swelling and minimizes discomfort.
- Rest: Adequate rest allows the body to heal more efficiently. Avoiding strenuous activities and excessive exertion is crucial.
- Hydration: Drinking plenty of fluids promotes healing and helps to flush out toxins.
- Gentle Cleansing: Carefully cleaning the nasal area with a soft cloth and saline solution as directed by the surgeon helps maintain hygiene and prevents infection.
Complications Causing Increased Pain and Discomfort, How bad do nose jobs hurt
While most rhinoplasty patients experience manageable post-operative pain, certain complications can lead to increased discomfort. These include:
- Infection: A nasal infection can cause significant pain, swelling, and fever. Early detection and treatment with antibiotics are essential.
- Hematoma: A collection of blood within the nasal tissues can cause significant pressure and pain. This often requires drainage by the surgeon.
- Septal Hematoma: A specific type of hematoma affecting the nasal septum (the cartilage dividing the nostrils) can cause severe pain and potentially lead to septal perforation if left untreated. This requires immediate medical attention.
- Sinusitis: Inflammation of the sinuses can lead to headaches and facial pain, potentially exacerbating post-operative discomfort.
- Poor Wound Healing: Delayed or impaired wound healing can prolong pain and increase the risk of infection. This may necessitate further surgical intervention.
Pain Management Strategies
Effective pain management is crucial for a comfortable recovery after rhinoplasty. A multi-modal approach, combining medication and self-care techniques, is generally recommended to minimize discomfort and promote healing. The specific strategies will be tailored to the individual patient’s needs and pain tolerance.
Medication Options for Pain Relief
Several types of medication are commonly prescribed to manage post-rhinoplasty pain. These range from over-the-counter analgesics to stronger prescription options, depending on the severity of the pain. Careful consideration of potential side effects and interactions with other medications is essential.
- Over-the-Counter Analgesics: Acetaminophen (Tylenol) is often recommended for mild to moderate pain. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil, Motrin) can help reduce both pain and swelling, but should be used cautiously due to potential bleeding risks in the post-operative period. Always consult your surgeon before taking any medication, including over-the-counter options.
- Prescription Pain Relievers: For more severe pain, your surgeon may prescribe stronger opioid pain relievers. These medications are typically used for a short duration due to the risk of dependence and side effects like constipation and drowsiness. The surgeon will carefully monitor the patient’s pain levels and adjust the medication as needed.
Importance of Following Post-Operative Instructions
Adherence to the surgeon’s post-operative instructions is paramount for minimizing pain and complications. These instructions often include specific guidelines for medication, ice application, elevation of the head, and activity restrictions. Failure to follow these instructions can lead to increased pain, swelling, and even complications that could delay recovery.
Sample Pain Management Plan
A typical pain management plan might include:
- Days 1-3: Prescription opioid pain medication as prescribed by the surgeon, taken every 4-6 hours as needed for pain. Ice packs applied to the nose for 15-20 minutes at a time, every 2-3 hours. Elevation of the head with extra pillows while sleeping.
- Days 4-7: Gradual reduction in opioid medication, transitioning to acetaminophen or ibuprofen as pain subsides. Continue ice application as needed. Gentle cleansing of the nasal area as instructed by the surgeon.
- Days 7-14: Continue with over-the-counter pain relievers as needed. Focus on gentle activities and avoid strenuous exercise. Follow-up appointment with the surgeon to assess healing progress.
Note: This is a sample plan and individual plans may vary significantly based on individual responses to surgery and pain tolerance.
Comparison of Pain Relief Options
| Pain Relief Option | Advantages | Disadvantages |
|---|---|---|
| Acetaminophen | Readily available, generally safe | Less effective for inflammatory pain |
| Ibuprofen | Reduces pain and inflammation | Potential bleeding risk, gastrointestinal side effects |
| Prescription Opioids | Effective for severe pain | Risk of dependence, constipation, drowsiness, nausea |
Patient Experiences and Testimonials
Patient experiences with rhinoplasty pain vary significantly, highlighting the subjective nature of pain perception and the influence of individual factors. Understanding these variations is crucial for managing patient expectations and providing appropriate pain management strategies. The following examples illustrate this variability. It is important to remember that these are fictionalized examples for illustrative purposes and do not represent the experience of any specific individual.
Patient Testimonials and Pain Variability
The table below presents fictionalized patient testimonials, demonstrating the range of pain experiences following rhinoplasty. Pain levels are subjective and reported on a scale of 1 to 10, with 1 being no pain and 10 being the worst imaginable pain. Recovery time is also highly individual and dependent on various factors including the complexity of the surgery and the patient’s healing process.
| Patient ID | Pain Level (Scale 1-10) | Pain Management Used | Recovery Time |
|---|---|---|---|
| P1 | 3-4 (primarily during the first 24 hours) | Over-the-counter pain relievers (ibuprofen) | 2 weeks (minimal bruising and swelling) |
| P2 | 6-7 (peak pain on day 2-3) | Prescription pain medication (opioids for initial days, then ibuprofen) | 4 weeks (moderate bruising and swelling) |
| P3 | 1-2 (minimal discomfort) | None required | 1 week (minimal bruising and swelling) |
| P4 | 8-9 (severe pain in the first 48 hours) | Prescription pain medication (opioids and other analgesics) | 6 weeks (significant bruising and swelling) |
Surgeon Advice on Managing Patient Expectations
Experienced surgeons emphasize the importance of open communication with patients to manage expectations regarding post-operative pain. They often explain that while some discomfort is expected, the severity and duration of pain vary widely. Surgeons typically discuss various pain management options available and emphasize the importance of adhering to post-operative instructions to minimize discomfort and promote healing. They might advise patients to prepare for potential pain by stocking up on prescribed and over-the-counter pain medications beforehand.
The surgeon’s role is not only to perform the surgery skillfully but also to provide comprehensive pre- and post-operative care, including realistic pain management expectations. This helps alleviate anxiety and fosters a positive patient experience.
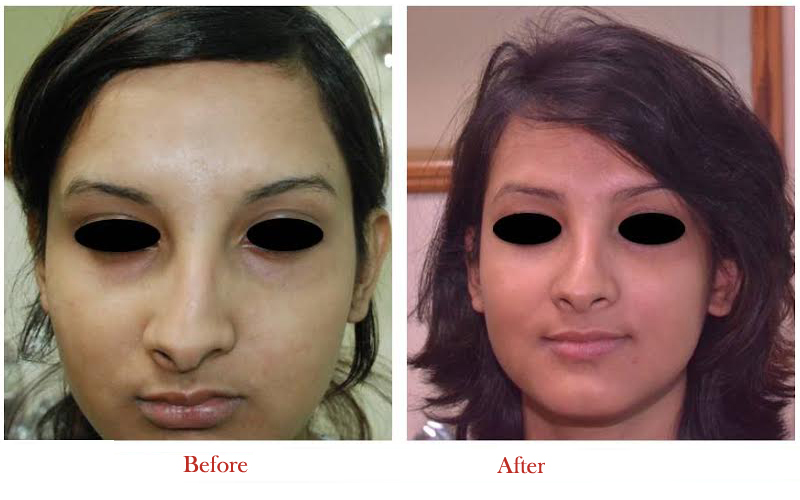
Visual Representations of Pain and Swelling

Rhinoplasty, while transformative, involves a period of recovery marked by both swelling and potential discomfort. Understanding the visual manifestations of these post-operative effects can help patients manage expectations and better understand their healing progress. The following descriptions aim to provide a realistic picture of what to expect.
Swelling and Bruising After Rhinoplasty
Post-operative swelling is a normal and expected part of the healing process. Immediately following surgery, the nose and surrounding areas will appear significantly swollen, often accompanied by bruising. The swelling is most pronounced in the first few days, gradually diminishing over several weeks. Bruising typically appears as discoloration, ranging from light purple to deep blue or black, depending on the individual and the extent of the surgery.
The severity of both swelling and bruising varies considerably between patients. In some individuals, swelling might be minimal, while others may experience more pronounced edema extending to the cheeks and around the eyes. Bruising typically resolves within two weeks, though discoloration may linger for a longer period. Over the course of several weeks, the swelling will gradually decrease, with the nose’s shape becoming progressively clearer and more defined.
At approximately six months post-surgery, the majority of swelling will have subsided, although subtle changes may continue for up to a year. A patient might initially present with a significantly enlarged and distorted nasal shape, with extensive purple and black bruising extending down the cheeks. A week later, the bruising might have faded to a yellowish hue, and the swelling would be noticeably reduced.
By one month post-op, the swelling would be significantly less, and the nose’s shape would be more readily apparent, although still somewhat swollen.
Facial Expressions Indicating Pain Levels
The intensity of pain experienced after rhinoplasty is subjective and varies widely. However, certain facial expressions and body language cues can provide some indication of the level of discomfort a patient is experiencing. A patient experiencing mild discomfort might exhibit slight wincing or a furrowed brow, perhaps accompanied by gentle touching of the nose. More significant pain might be indicated by a more pronounced grimace, closed eyes, and possibly a rigid posture or avoidance of movement.
In cases of severe pain, a patient may display more dramatic facial expressions, including a clenched jaw, and exhibit signs of distress such as shallow breathing or restlessness. It’s important to note that these are general observations and should not be interpreted as definitive indicators of pain intensity without considering other factors, such as the patient’s individual pain tolerance and communication abilities.
For example, one patient might display a significant grimace with mild pain, while another might show little outward expression of even severe discomfort.
Last Word
Ultimately, the pain associated with a nose job is subjective and variable. While discomfort is expected, effective pain management techniques are readily available to minimize suffering. Understanding the factors influencing pain perception, such as individual tolerance and the type of surgery performed, allows for better preparation and realistic expectations. Open communication with your surgeon and proactive self-care strategies are essential for a smoother recovery process.
Remember, while some discomfort is normal, severe or persistent pain should always be addressed promptly with your medical team.
