How are dental implants removed? This question, while seemingly straightforward, encompasses a complex surgical procedure with various considerations. Understanding the reasons for removal, the intricacies of the surgical process itself, and the potential complications is crucial for both patients and dental professionals. This comprehensive overview explores the different types of implants, removal techniques, post-operative care, and alternative treatment options following implant extraction.
The process begins with a thorough assessment of the implant’s condition and the patient’s overall health. Specialized instruments are employed to carefully section and remove the implant, minimizing damage to surrounding bone and soft tissues. The procedure’s complexity varies depending on factors such as the type of implant, its osseointegration level, and the presence of any complications. Post-operative care is critical for successful healing and minimizing the risk of infection or other adverse effects.
Reasons for Dental Implant Removal: How Are Dental Implants Removed
Dental implant removal, while less common than placement, is sometimes necessary due to a variety of factors. These factors can broadly be categorized into medical reasons, complications arising from the implant itself, restorative needs, and underlying patient health issues. Understanding these reasons is crucial for both patients and dental professionals to make informed decisions regarding implant management.
Medical Reasons for Dental Implant Removal
Certain medical conditions can necessitate the removal of dental implants. For example, a patient developing a severe systemic illness that compromises their immune system might require implant removal to minimize the risk of infection. Similarly, patients undergoing radiation therapy to the head and neck region may experience compromised bone health around the implant, making removal necessary to prevent complications.
In cases of uncontrolled diabetes, the healing process might be severely impaired, potentially leading to implant failure and the need for removal. The decision to remove an implant in these situations is based on a comprehensive assessment of the patient’s overall health and the potential risks associated with retaining the implant.
Infections and Complications Related to Dental Implant Removal
Peri-implantitis, a serious infection around the dental implant, is a primary reason for implant removal. This infection can lead to bone loss, inflammation, and pain. If conservative treatment methods, such as antibiotics and professional cleaning, fail to resolve the infection, implant removal may be the only option to prevent further damage and systemic complications. Other complications, such as implant fracture or loosening due to trauma or excessive stress, might also necessitate removal.
In these cases, the damaged implant needs to be removed to prevent further issues and allow for potential replacement with a new, properly placed implant.
Restorative Reasons for Dental Implant Removal
Sometimes, an implant may need removal for restorative reasons, even if it is otherwise healthy. This can occur if a new restoration (such as a crown) cannot be successfully placed on the existing implant due to unforeseen technical difficulties during placement or subsequent damage. In such cases, removing the implant allows for a more optimal approach to restoring the missing tooth, potentially with a different implant design or placement technique.
Similarly, if the original implant placement was compromised, leading to an improper position or angle, removal may be necessary to achieve a better aesthetic or functional outcome. This is especially relevant in the anterior region where aesthetics are of prime importance.
Patient Health Issues Requiring Implant Removal
Certain patient health issues can indirectly necessitate implant removal. For example, a patient who develops a severe allergy to the implant material may experience chronic inflammation and discomfort, necessitating its removal. Furthermore, patients undergoing major surgeries or procedures may require the removal of their dental implants to minimize risks during anesthesia or to ensure proper healing. In these situations, the implant is removed temporarily or permanently depending on the severity of the health issue and the patient’s overall prognosis.
Procedure for Dental Implant Removal
Dental implant removal is a surgical procedure requiring precision and expertise. The complexity varies depending on the implant’s condition, integration with the bone, and the presence of any complications. This section details the steps involved, the instruments used, and crucial considerations for both the procedure and patient recovery.
Surgical Steps in Dental Implant Removal
The removal of a dental implant is a multi-step process that often involves careful sectioning and removal of the implant components. Success depends heavily on the surgeon’s skill and the use of appropriate instruments.
| Step | Procedure | Instruments | Considerations |
|---|---|---|---|
| 1. Assessment and Planning | A thorough examination of the implant site, including radiographic imaging (X-rays, CBCT scans), is conducted to assess the implant’s position, bone level, and surrounding tissues. A treatment plan is developed based on this assessment. | Radiographic equipment (X-ray machine, CBCT scanner), periodontal probes, surgical mirrors | Accurate assessment is crucial for planning the surgical approach and minimizing complications. The patient’s medical history should be thoroughly reviewed. |
| 2. Anesthesia | Local anesthesia is typically administered to numb the area. In some cases, sedation or general anesthesia may be used, depending on the patient’s needs and the complexity of the procedure. | Local anesthetic solution, sedation medication (if applicable), general anesthesia equipment (if applicable) | Patient comfort and safety are paramount. The type of anesthesia should be carefully chosen based on individual patient factors and the surgeon’s judgment. |
| 3. Incision and Exposure | A small incision is made in the gum tissue to expose the implant. The surgeon carefully dissects the soft tissues to gain access to the implant fixture. | Scalpel, surgical scissors, retractors, periosteal elevators | Minimizing tissue trauma is crucial for optimal healing. Careful dissection prevents damage to surrounding structures. |
| 4. Implant Sectioning (if necessary) | If the implant is firmly integrated into the bone, it may need to be sectioned into smaller pieces using specialized instruments to facilitate removal. This step is not always necessary. | Surgical burs, ultrasonic scalers, implant removal instruments (e.g., osteotomes) | Precise sectioning is essential to avoid damage to adjacent teeth or bone. Careful control of force is necessary to prevent fracture of the implant or surrounding bone. |
| 5. Implant Removal | Once the implant is sectioned (if applicable), specialized instruments are used to carefully loosen and remove the implant fixture from the bone. | Implant removal forceps, osteotomes, elevators | Gentle force and controlled movements are critical to avoid fracture of the implant or damage to the surrounding bone. |
| 6. Bone Assessment and Debridement | The bone socket is carefully examined for any residual implant fragments, and any damaged or infected bone is removed (debridement). | Curettes, surgical burs, irrigation system | Thorough debridement is crucial to prevent infection and promote healing. |
| 7. Wound Closure | The incision is closed with sutures, and the area is thoroughly cleaned and dressed. | Surgical sutures, antiseptic solution, sterile dressing | Proper wound closure minimizes scarring and reduces the risk of infection. |
| 8. Post-Operative Instructions | The patient receives detailed instructions on post-operative care, including pain management, oral hygiene, and follow-up appointments. | Post-operative care instructions, pain medication prescriptions | Adherence to post-operative instructions is crucial for optimal healing and to prevent complications. |
Specialized Instruments Used in Dental Implant Removal
A variety of specialized instruments are used during dental implant removal, designed to minimize trauma and maximize efficiency. These include but are not limited to: osteotomes (for bone removal and implant sectioning), specialized forceps designed to grip and remove implant fixtures, ultrasonic scalers (for removing bone debris), and various burs and drills for sectioning the implant. The choice of instruments depends on the specific clinical situation.
Types of Implants and Removal Techniques
Dental implant removal is a procedure that varies significantly depending on the type of implant and the degree of osseointegration (the bonding of the implant to the jawbone). Understanding these factors is crucial for planning a safe and effective removal. Different implant materials and designs present unique challenges during the extraction process.
The success of implant removal hinges on careful assessment of the implant’s characteristics and the patient’s overall health. Factors such as implant age, bone density, and the presence of complications all influence the chosen technique. While some removals are straightforward, others require specialized instruments and techniques to minimize the risk of damage to surrounding tissues and bone.
Implant Material and Removal Methods
The material of the implant significantly impacts the removal process. Titanium, the most common material, is biocompatible and strong, but its robust nature can make removal challenging. Other materials, such as zirconia, may exhibit different properties affecting the ease of extraction.
The techniques employed are largely determined by the material’s characteristics and the degree of osseointegration. For instance, highly osseointegrated titanium implants often require specialized instruments and potentially surgical techniques to avoid fracture.
- Titanium Implants: These implants, being the most common, often require the use of specialized removal instruments, such as ultrasonic devices or osteotomes, to section the implant into smaller pieces for easier extraction. Excessive force can lead to implant fracture or damage to the surrounding bone. In cases of significant osseointegration, surgical sectioning may be necessary.
- Zirconia Implants: While possessing excellent biocompatibility, zirconia implants can be brittle and prone to fracture under excessive force during removal. Therefore, careful consideration and precise techniques are crucial. Ultrasonic instruments are often preferred to minimize the risk of fracture.
- Other Materials: Less common implant materials may necessitate individualized approaches based on their specific properties. Pre-operative assessment and planning are paramount to ensure a safe and successful removal.
Osseointegration Level and Removal Challenges
The degree of osseointegration—the extent to which the implant has fused with the jawbone—is a critical factor determining the complexity of removal. Highly osseointegrated implants require more aggressive techniques and specialized instruments.
Low osseointegration implies a less secure bond between the implant and bone, making removal relatively easier. Conversely, high osseointegration presents a significant challenge, potentially requiring sectioning of the implant to facilitate removal. This is to prevent damage to the surrounding bone structure and adjacent teeth.
- Low Osseointegration: Removal is generally less challenging and may be accomplished with simpler instruments and less invasive techniques.
- High Osseointegration: Removal often requires more advanced techniques, including the use of specialized instruments like ultrasonic devices or surgical drills to section the implant. The risk of implant fracture and bone damage is higher in these cases.
Specific Removal Techniques
The selection of a removal technique depends on several factors, including the implant type, osseointegration level, and the presence of any complications. Careful planning and consideration of these factors are essential for a successful outcome.
Several techniques exist, each tailored to specific circumstances. The goal is always to remove the implant while preserving the surrounding bone and minimizing patient discomfort and complications.
- Osteotomy: This involves surgically removing the bone surrounding the implant to gain access and facilitate removal.
- Sectioning: The implant is cut into smaller pieces using specialized instruments to ease extraction.
- Ultrasonic Removal: High-frequency vibrations are used to loosen the implant from the bone, minimizing trauma.
- Surgical Extraction: A more invasive procedure that may be necessary for complex cases involving significant osseointegration or complications.
Potential Complications and Risks
Dental implant removal, while generally a safe procedure, carries potential complications and risks. The severity of these complications can vary depending on factors such as the type of implant, the patient’s overall health, and the skill of the surgeon. Understanding these potential issues is crucial for informed consent and effective post-operative management.
Types of Complications
Several complications can occur during or after dental implant removal. These complications can range from minor discomfort to serious health issues requiring further intervention. Careful planning and execution of the procedure, coupled with diligent post-operative care, are essential for minimizing these risks.
Nerve Damage
Dental implants are often situated close to nerves responsible for sensation in the jaw and face. During removal, there is a risk of damaging these nerves, leading to numbness, tingling, or pain in the affected area. This risk is higher with implants placed in close proximity to major nerves. The severity of nerve damage can range from temporary paresthesia (numbness or tingling) that resolves spontaneously to permanent nerve damage requiring extensive rehabilitation.
Careful surgical planning, using advanced imaging techniques like CBCT scans, and meticulous surgical technique are essential to minimize this risk.
Infection
Infection is a significant potential complication of dental implant removal. Bacteria can enter the surgical site, leading to localized inflammation, pain, and swelling. In severe cases, infection can spread to surrounding tissues, causing osteomyelitis (bone infection) or even systemic infection. Prophylactic antibiotics are often prescribed before and after the procedure to reduce the risk of infection. Maintaining meticulous oral hygiene post-operatively is crucial in preventing infection.
Fracture of the Jawbone
In some cases, particularly with osseointegrated implants, the removal process may cause a fracture of the surrounding jawbone. This risk is higher with implants that have been in place for a long time or those that have experienced significant bone loss. Pre-operative assessment using radiographic imaging can help identify potential risks of jawbone fracture. Careful surgical technique and the use of appropriate instruments are essential to minimize this complication.
Sinus Perforation
Implants placed in the maxillary (upper) jaw are close to the maxillary sinus. During removal, there is a risk of perforating the sinus membrane, which can lead to a communication between the oral cavity and the sinus. This can result in sinusitis, pain, and potentially require additional surgical intervention to repair the perforation. Careful surgical planning and meticulous technique are vital to avoid this complication.
Hemorrhage
Bleeding is a potential complication during any surgical procedure, including dental implant removal. While usually minor, significant hemorrhage can occur, particularly in patients with bleeding disorders or those taking anticoagulant medications. Pre-operative assessment of the patient’s medical history and careful surgical technique, including meticulous hemostasis (stopping bleeding), are crucial in minimizing this risk.
Strategies for Minimizing Risks and Complications
Careful patient selection and pre-operative planning are paramount. This includes a thorough medical history review, radiographic imaging (such as panoramic radiographs and CBCT scans) to assess the implant position and bone density, and a discussion of potential risks and complications with the patient. Selecting experienced and qualified surgeons with expertise in implant removal is crucial. The use of advanced surgical techniques and instrumentation can further minimize complications.
Post-operative Care to Prevent Complications, How are dental implants removed
Post-operative instructions should be followed meticulously. This includes maintaining meticulous oral hygiene, using prescribed medications (such as antibiotics and pain relievers), avoiding strenuous activities, and following a soft food diet for the initial healing period. Regular follow-up appointments with the dentist are crucial to monitor healing and address any potential complications promptly. Prompt attention to any signs of infection (such as increasing pain, swelling, or redness) is essential to prevent serious complications.
Post-Removal Care and Healing
Post-operative care following dental implant removal is crucial for proper healing and minimizing complications. The healing process involves the body’s natural repair mechanisms, including blood clot formation, tissue regeneration, and bone remodeling. Careful adherence to the dentist’s instructions is essential for a successful outcome.
The initial post-operative period is characterized by some degree of swelling, pain, and bleeding. These symptoms are typically managed with prescribed pain medication, ice packs applied to the affected area, and gentle rinsing with saltwater. The intensity and duration of these symptoms vary depending on the complexity of the procedure and individual patient factors. Proper nutrition, including soft foods, is also important to aid healing and prevent discomfort during chewing.
Expected Symptoms and Their Management
Following dental implant removal, patients can expect a range of symptoms. Swelling is common and usually peaks within 24-48 hours. Pain is managed with prescribed analgesics such as ibuprofen or stronger medications if necessary. Bleeding is usually minimal and can be controlled with gentle pressure using a gauze pad. A slight fever is also possible and should resolve within a few days.
Persistent or worsening symptoms should be reported to the dentist immediately. For example, a patient experiencing severe pain not relieved by medication or excessive bleeding should seek immediate medical attention. This proactive approach ensures timely intervention and prevents potential complications.
Maintaining Oral Hygiene After Implant Removal
Maintaining meticulous oral hygiene is paramount during the healing process. Gentle brushing and rinsing with a prescribed antiseptic mouthwash are crucial to prevent infection and promote healing. Avoid vigorous brushing or flossing near the extraction site to prevent dislodging the blood clot. Instead, focus on gently cleaning surrounding areas. Regular rinsing with warm salt water can help keep the area clean and reduce inflammation.
A diet of soft foods will minimize irritation and trauma to the healing site. For instance, a patient might consume smoothies, yogurt, and mashed potatoes for the first few days. Consistent adherence to these guidelines minimizes the risk of complications such as dry socket.
Healing Timeline and Potential Complications
The healing process typically involves several stages. Immediate post-operative healing involves blood clot formation at the extraction site, which usually takes about 3-5 days. The socket then begins to fill with granulation tissue, a process that takes several weeks. Bone remodeling, the process where new bone replaces the lost bone, can take several months. Complete healing, however, can take up to six months or longer, depending on individual factors and the complexity of the removal.
Potential complications include dry socket (alveolar osteitis), infection, and nerve damage. Dry socket occurs when the blood clot is dislodged from the extraction site, exposing the underlying bone. This is typically characterized by severe pain, bad breath, and a visible empty socket. Treatment involves irrigation of the socket and placement of a medicated dressing. Infection can manifest as increased pain, swelling, and pus formation.
Antibiotics are typically prescribed to treat infection. Nerve damage, although rare, can result in numbness or tingling in the affected area. This usually resolves over time, but in some cases, may require further intervention. For instance, a patient experiencing persistent numbness after several months post-surgery might require further evaluation by a specialist.
Alternative Treatment Options After Removal
Dental implant removal necessitates consideration of subsequent treatment options to restore oral function and aesthetics. The choice depends on various factors, including the reason for removal, the remaining dentition, and the patient’s overall health and financial resources. Several alternatives exist, each with its own advantages and disadvantages.
Treatment Options Following Dental Implant Removal
After a dental implant is removed, several options exist to address the resulting gap in the dentition. These options range from leaving the space empty to utilizing more complex restorative techniques. The best option depends on the individual patient’s needs and circumstances.
Comparison of Treatment Options
The following table compares different treatment options available after dental implant removal, considering cost, recovery time, and longevity. Cost estimates are broad ranges and can vary significantly based on location, complexity of the procedure, and the materials used. Recovery times are also approximate and depend on individual healing rates and the specific procedure.
Dental implant removal involves a surgical procedure, often requiring the dentist to section the implant for easier extraction. The process is significantly different from, say, determining the correct number of spacers for a 1992 Corvette’s rear monospring, as detailed on this helpful resource: 1992 vette rear monspring how many spacer. Similarly, precise surgical techniques are crucial for successful dental implant removal to minimize trauma and ensure proper healing.
| Treatment Option | Description | Cost | Recovery Time | Longevity | Advantages | Disadvantages |
|---|---|---|---|---|---|---|
| Leaving the Space Empty | No further treatment is undertaken. | $0 | None | N/A | Least invasive, inexpensive. | May affect adjacent teeth, aesthetics compromised, impaired chewing function. |
| Removable Partial Denture | A partial denture replaces the missing tooth. | $500 – $2000 | Minimal | 5-10 years (with regular maintenance) | Relatively inexpensive, easily removable for cleaning. | Can be uncomfortable, may affect speech, requires regular cleaning and maintenance. |
| Fixed Partial Denture (Bridge) | A bridge is cemented to adjacent teeth. | $1500 – $5000 | 1-2 weeks | 10-15 years (with good oral hygiene) | Natural-looking, good chewing function. | Requires preparation of adjacent teeth, cannot be removed for cleaning. |
| New Dental Implant | Placement of a new dental implant. | $3000 – $7000+ per implant | Several months (including healing and restoration) | 20+ years (with good oral hygiene) | Most natural-looking and functional option, long-lasting. | Most expensive, longer recovery time, potential for complications. |
Factors Influencing Treatment Choice
Several factors influence the choice of treatment after dental implant removal. These include the patient’s overall health, the reason for implant removal (e.g., infection, failure), the number of remaining teeth, the patient’s financial resources, and aesthetic concerns. For example, a patient with extensive periodontal disease might be a poor candidate for a new implant, whereas a patient with good oral hygiene and financial resources might prefer this option for its longevity and aesthetics.
Similarly, a patient with limited financial resources might opt for a removable partial denture as a more affordable solution.
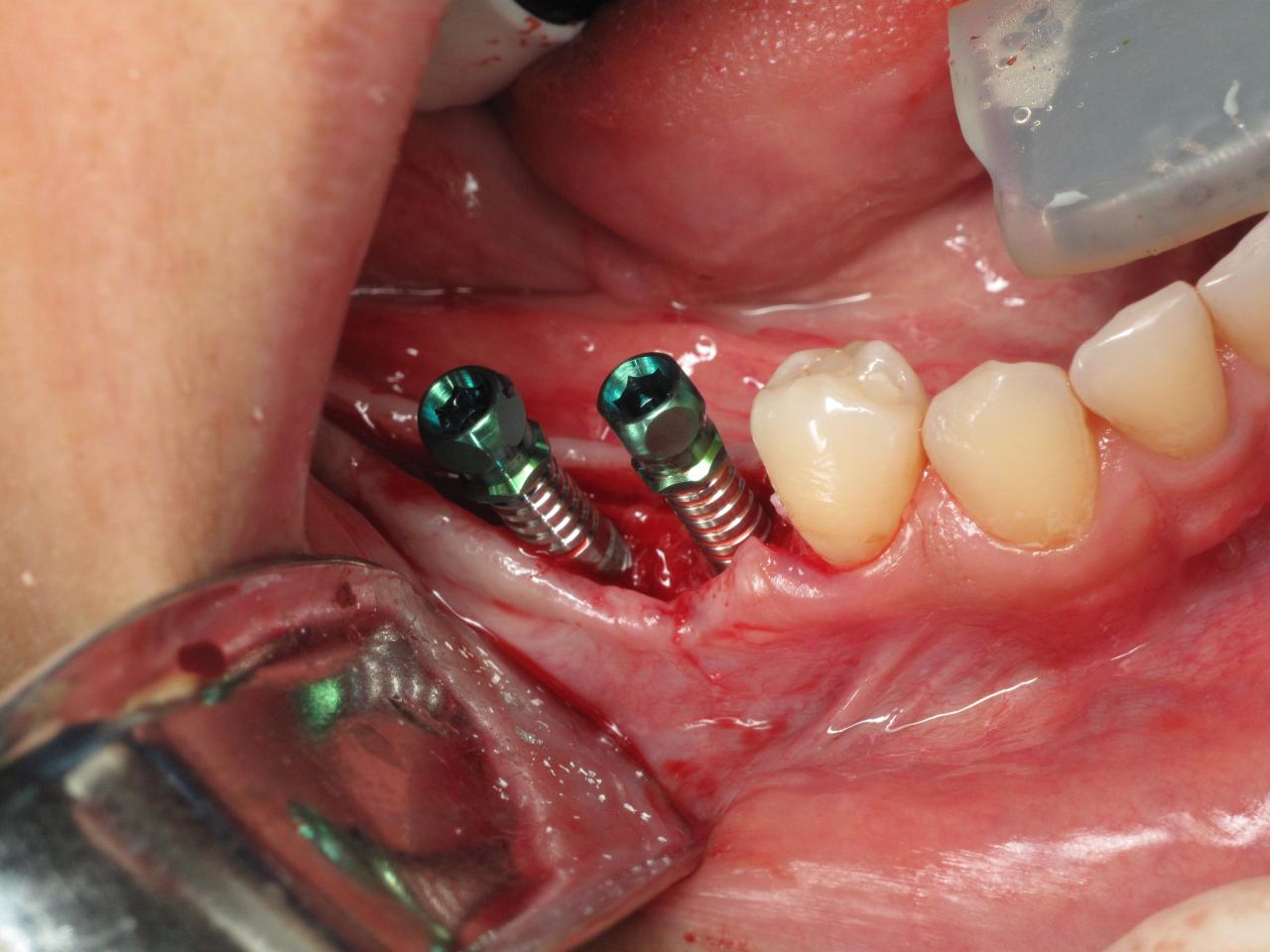
Visual Representation of the Removal Process
Dental implant removal is a surgical procedure requiring precision and a thorough understanding of the implant’s integration with the surrounding bone and soft tissues. Visualizing the process helps understand the steps involved and potential challenges. The following description focuses on the interaction between surgical instruments, the implant, and the surrounding alveolar bone and gingiva.The process begins with a thorough assessment of the implant’s position and the surrounding bone density using radiographic imaging (like a periapical radiograph or CBCT scan).
This allows the surgeon to plan the optimal approach for removal, minimizing damage to adjacent teeth and structures. The initial incision is made in the gingiva, carefully reflecting the soft tissue flap to expose the implant fixture. This involves precise manipulation of delicate tissues to gain access without unnecessary trauma. The surgeon uses a variety of instruments, carefully chosen based on the implant type and its integration with the bone.
Surgical Instruments and Their Functions
The removal process typically involves a series of specialized instruments. First, a small incision is made in the gingiva using a scalpel or electrosurgical unit. Retractors are then used to gently hold back the soft tissues, providing clear access to the implant. Depending on the type of implant, the surgeon might use a specialized implant removal instrument, such as a forceps or a drill.
Forceps are used to grip and remove the implant, while drills may be needed to section or loosen the implant before removal. In cases where the implant is firmly integrated, an ultrasonic device may be employed to help break down the bone-implant interface. Throughout the procedure, copious irrigation with saline solution is used to remove debris and maintain a clear surgical field.
Bone files or curettes might be used to smooth any irregularities in the bone after implant removal. Finally, the soft tissue is meticulously repositioned and sutured closed.
Bone and Soft Tissue Interactions During Removal
The success of implant removal depends on careful consideration of the interaction between the surgical instruments and the surrounding bone and soft tissues. The implant itself is usually made of titanium, a biocompatible material that integrates with the bone over time. This integration, called osseointegration, is what provides stability to the implant. During removal, the surgeon needs to carefully separate the implant from the surrounding bone without causing excessive bone loss or damage to adjacent structures such as the maxillary sinus or the mandibular nerve.
The removal process can involve careful sectioning of the implant, especially in cases where the implant is deeply seated or has significant bone integration. This minimizes the risk of fracturing the surrounding bone during extraction. The soft tissue, particularly the gingiva, is handled gently throughout the process to minimize trauma and promote healing. The careful repositioning of the soft tissues is crucial for optimal wound closure and to prevent complications like infection or excessive scarring.
Example of a Specific Implant Removal
Consider a scenario involving a Branemark-type endosseous implant. The initial incision would expose the implant head. A specialized implant removal wrench or forceps would then be used to grip the implant and apply controlled force. Depending on the level of osseointegration, the implant might be removed relatively easily or may require sectioning using a small drill. In the case of significant osseointegration, ultrasonic bone surgery may be required to carefully break down the bone-implant interface.
Once the implant is removed, the surgeon would assess the extraction site for any bone defects or irregularities. Bone grafting material might be used to fill any bone defects before closing the wound.
Final Summary
Dental implant removal, while a relatively uncommon procedure, requires precision and expertise. Understanding the reasons for removal, the various techniques involved, and the potential complications is vital for a successful outcome. Careful planning, meticulous execution, and diligent post-operative care are key to minimizing risks and ensuring optimal patient recovery. The choice of subsequent treatment will depend on individual needs and preferences, with various options available to restore function and aesthetics.
